
Beta lactam allergy cross reactivity chart skin#
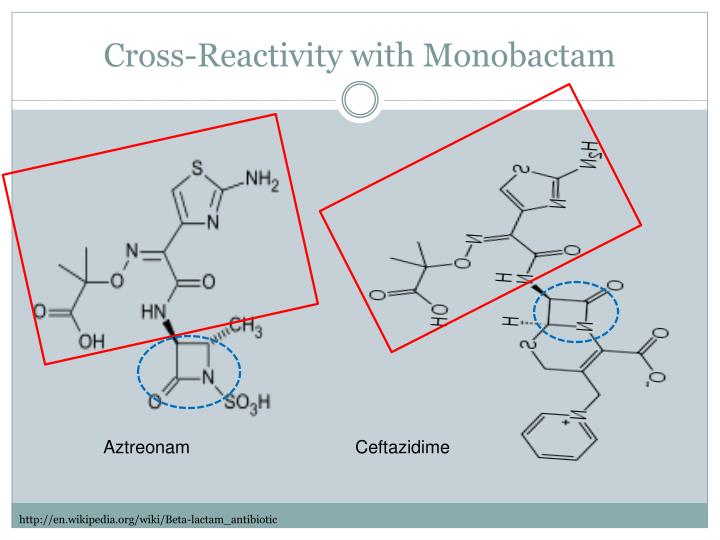
80% of patients who tested positive for a penicillin allergy via penicillin skin test and 60% who tested positive for a cephalosporin allergy via cephalosporin skin test are no longer positive after 10 and 5 years, respectively. This is important not just because of misclassification but because IgE-mediated reactions to beta – lactams may self-resolve over time. Several studies suggest that 75% of penicillin allergy labels are obtained by the age of three and are either not truly allergic in nature, low risk for immediate hypersensitivity, or are a potential antibody-mediated reaction that may have waned over time. It is expected that the incidence of true beta-lactam allergies in children is low. These adverse drug reactions are not true allergies and may prevent a patient from receiving a beta-lactam antibiotic.Ĭhildren may have had an observed allergic reaction to a beta-lactam however, it is likely the observed reaction was related to a viral exanthem rather than the medication itself. This is concerning because it could be an unverified allergy that is recorded in the patient’s chart incorrectly after a non-immunologic reaction such as nausea, headache, or fatigue. It is common to encounter patients in the ED with an indicator on their profile for penicillin allergy and much of the time the reaction type is undocumented. Beta-lactam adverse drug reactions are documented in up to 15% of patient charts, and these reactions often go unverified, resulting in avoidance of the drug class. Beta-lactam antibiotics, which include penicillins, cephalosporins, carbapenems, and monobactams, are the most common antibiotic class implicated in hypersensitivity reactions.


 0 kommentar(er)
0 kommentar(er)
